Day 2 :
- Infection Control and Epidemiology | New or Rapid Diagnostics | Infection and Immune System | Nosocomial Infections | New Opportunities for Tuberculosis Control
Location: Barcelona, Spain
Session Introduction
Imran Khan
University of California, Davis, USA
Title: Disease biomarkers for studies on tuberculosis (TB) and TB diagnostic applications

Biography:
Imran H Khan completed his PhD (Molecular & Cellular Biology) at Albert Einstein College of Medicine, NY. His research program has focused on “Infectious diseases, intracellular signaling pathways, molecular biology” for over 15 years. Since 2002, he has worked on developing highly efficient and high throughput multiplex approaches for infectious disease biomarkers (e.g., tuberculosis). His research includes simultaneous analysis of multiple key components of cell signaling pathways in a single reaction vessel. In addition, he has employed novel approaches to study disease related biomarkers (e.g., immune biomarkers) in bodily fluids (e.g., plasma/serum) by combining the power of multiplexing systems and computational modeling. Results of his research have been published in peer reviewed journals for the development of novel methods for biomarker profiling for cancer, inflammatory diseases and infectious diseases.
Abstract:
Approximately, two billion people worldwide are infected with Mycobacterium tuberculosis (M. tb.), the etiologic agent of tuberculosis (TB). A tenth of the infected individuals develop active disease. Active pulmonary TB is an inflammatory disease and is increasingly viewed as an imbalance of host immune responses to M. tb. infection. The current frontline diagnostic methods including sputum smear (SS) microscopy and X-ray are insensitive, inefficient, cumbersome or too expensive. The most widely used test, SS microscopy (WHO standard) test has a low sensitivity. Therefore, there is an urgent need for low cost, efficient, high-throughput and accurate diagnostic approaches. We have developed multiplex antibody biomarker based TB diagnostic system. Data from proof-of-concept and subsequent field studies have shown that this approach will enable a scalable, flexible and cost effective model for diagnostic applications. In addition, we have published 10 plasma cytokine/chemokine biomarkers representing host immune-responses in TB patients, are not only gender biased but concentrations of some of these biomarkers (e.g., IP-10, MIG, IL-16, IFN-α and G-CSF) progressively decreased in patients which responded to anti-tuberculosis treatment (ATT) with a cocktail of several drugs (isoniazid, rifampin, ethambutol, and pyrazinamide or streptomycin-WHO standard). These decreases strongly correlated treatment success and can be used for monitoring efficacy of therapy. This is important because ATT is a drawn out process (at least six months), and early detection of patients who may not respond to therapy is important. One possible reason for not responding to ATT could be due to infection with multi-drug resistant (MDR) strain of M. tb. The standard culture based drug sensitivity testing can take several weeks. Therefore, there is a need for rapid molecular tests. A test, based on multiplex gene amplification (multiplex PCR), of several M. tb. genes involved in drug resistance, and multiplex detection of the relevant gene mutations to detect resistance against four TB drugs will also be discussed.
Approximately, two billion people worldwide are infected with Mycobacterium tuberculosis (M. tb.), the etiologic agent of tuberculosis (TB). A tenth of the infected individuals develop active disease. Active pulmonary TB is an inflammatory disease and is increasingly viewed as an imbalance of host immune responses to M. tb. infection. The current frontline diagnostic methods including sputum smear (SS) microscopy and X-ray are insensitive, inefficient, cumbersome or too expensive. The most widely used test, SS microscopy (WHO standard) test has a low sensitivity. Therefore, there is an urgent need for low cost, efficient, high-throughput and accurate diagnostic approaches. We have developed multiplex antibody biomarker based TB diagnostic system. Data from proof-of-concept and subsequent field studies have shown that this approach will enable a scalable, flexible and cost effective model for diagnostic applications. In addition, we have published 10 plasma cytokine/chemokine biomarkers representing host immune-responses in TB patients, are not only gender biased but concentrations of some of these biomarkers (e.g., IP-10, MIG, IL-16, IFN-α and G-CSF) progressively decreased in patients which responded to anti-tuberculosis treatment (ATT) with a cocktail of several drugs (isoniazid, rifampin, ethambutol, and pyrazinamide or streptomycin-WHO standard). These decreases strongly correlated treatment success and can be used for monitoring efficacy of therapy. This is important because ATT is a drawn out process (at least six months), and early detection of patients who may not respond to therapy is important. One possible reason for not responding to ATT could be due to infection with multi-drug resistant (MDR) strain of M. tb. The standard culture based drug sensitivity testing can take several weeks. Therefore, there is a need for rapid molecular tests. A test, based on multiplex gene amplification (multiplex PCR), of several M. tb. genes involved in drug resistance, and multiplex detection of the relevant gene mutations to detect resistance against four TB drugs will also be discussed.
Hailay Gesesew
Flinders University, Australia
Title: HIV care continuum outcomes: Does Ethiopia meet the UNAIDS 90-90-90 targets?

Biography:
Hailay Gesesew has his expertise in Epidemiology. His multi-method approach assessing in each cascades of HIV care continuum will establish a significant contribution for the AIDS ending goal. He has been publishing a lot of peer reviewed articles in the area of HIV Care in reputed journals. His publications produced from his PhD will improve the HIV care in developing countries especially Ethiopia. He has been serving as a Clinician, Academician and Researcher.
Abstract:
Background: How Ethiopia’s UNAIDS 90-90-90 targets is progressing was not assessed. We assessed HIV care continuum outcomes as surrogate markers for the 90-90-90 targets.
Methodology: Data were collected from a 12 years retrospective cohort from anti-retroviral therapy (ART) clinic in Southwest Ethiopia. For measuring the UNAIDS diagnosis target, prevalence rate of delayed HIV diagnosis was considered as a surrogate marker. For the treatment target, number of people on ART, number of people who discontinued from ART or transferred out, and number of people who had fair or poor adherence were used as surrogate markers. For the viral suppression target, number of CD4 counts and/or WHO clinical stages were used to assess immunological, clinical and treatment successes and further show the viral suppression. Summary statistics, trends and estimated survival time were reported.
Results: 8172 patients were enrolled for HIV cares in 2003-2015. For the diagnosis target, 34.5% patients knew their status early (43%-children, 33%-adults). For the treatment target, 65% patients received ART, 1154 (21.9%) patients discontinued from ART, 1015 (19.3%) patients on ART transferred out to other sites, 916 (17%) of patients on ART had fair or good adherence. For the virological suppression target, 80.7, 80.3 and 65.8% of patients had immunological, clinical and treatment success displaying an estimated 66% of patients achieved the target.
Conclusions: The finding reflects that an estimated 35% of patients knew their status timely, 65% of diagnosed patients received treatment and 66% of patients on ART achieved viral suppression. This is very far from the UNAIDS 90-90-90 targets underscoring the need for concreted efforts such as use of unmanned aerial systems (or drones) for transporting laboratory specimens, immediate or same day ART initiation, community distribution of ART, runaway packs during conflict, and use of GenXpert for HIV viral load testing would help to hit the target.
Ambak Kumar Rai
Motilal Nehru National Institute of Technology, India
Title: Characterization of phosphate transporter(s) and understanding their role in Leishmania donovani parasite

Biography:
Ambak Kumar Rai is an Assistant Professor in Department of Biotechnology at Motilal Nehru National Institute of Technology (MNNIT) Allahabad, India. He has his expertise in “Understanding the molecular and biochemical aspects of drug resistance in Leishmania donovani”. A detailed approach to understand the drug unresponsiveness offers new possibilities for therapeutic advancement. He is also inclined to understand the immuno-regulatory aspects of Leishmania pathogenesis.
Abstract:
Statement of the Problem: Inorganic phosphate (Pi) is shown to be involved in excretion of methylglyoxal (MG) in the promastigote form of Leishmania donovani parasite. Absence of Pi leads to its accumulation inside the parasite. Accumulation of MG is toxic to the parasite and utilizes glyoxalase as well as excretory pathways for its detoxification. In addition, Pi is also reported to regulate activities of ectoenzymes and energy metabolism (glucoseà pyruvate) etc. Thus, it cumulatively affects growth of the parasite. Therefore, the transporters which allow the movement of Pi across the membrane can prove to be a crucial drug target.
Methodology & Theoretical Orientation: Bioinformatics analysis approach was applied to identify the phosphate transporters in L. donovani. Phylogenetic analysis as well as secondary structure prediction was performed for its characterization. We tried to understand the secondary structure of these two proteins and confirm modulation in their expression with the change in Pi concentration outside. We also tried to detect the expression quantitatively in a log phase culture of promastigote and under various physiological conditions. Moreover, their modes of action were also measured in presence of different inhibitors (LiF, CCCP).
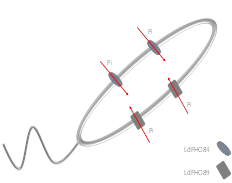
Findings: We first characterized two phosphate transporters in Leishmania: H+ dependent myo-inositol transporter PHO84 and; Na+ dependent transporter PHO89 based on similar studies done previously on other lower organisms and trypanosomatids. We found significantly higher expression of H+ dependent transporter (LdPHO84) as compared to Na+ dependent transporter (LdPHO89). We also inhibited the Na+ as well as H+ gradient and then confirmed their involvement in the Pi transport across the membrane.
Conclusion & Significance: We thus functionally characterized two phosphate transporters of L .donovani and its regulation by extracellular Pi for the first time. These computational results offer the possibility of identifying novel compounds which inhibit the transport of Pi across the membrane.
Oscar Gaunya
Busia County Referral Hospital, Kenya
Title: Cholera outbreak among residents of Bunyala in Busia county 2016
Biography:
Oscar Guanya is an expertise in emerging infectious diseases department working in Busia County Referral Hospital, Kenya
Abstract:
Background: Cholera is an acute enteric infection caused by the bacterium Vibrio cholerae of sero-groups 01 or 0139. It is water borne disease of public health importance with an estimated number of three to five million cases annually and 100,000 to 150,000 deaths yearly. Outbreaks are linked to consumption of unsafe water and food, poor hygiene and sanitation. Overflowing of latrines and contamination of wells and surface water, seasonal modification of water sources for consumption and human behavior may play a role in the occurrence of cholera outbreaks. Failure to control local outbreaks and prevention of between-region transmission could result in spread of cholera outbreaks to neighbouring regions or countries. The latest cholera outbreak in Bunyala Busia county is dated between 21st February to 11th March 2016. Though on the 1st January 2017, there were five confirmed cases reported in Uganda (Lumino village) who sought treatment at our County Referral Hospital Busia being at the boarder & then later transferred back to Uganda for further management. Cholera is one of the three diseases requiring notification to WHO under the International Health Regulations.
Aim: Aim of this study was to describe cholera outbreak by time, person and place.
Methodology: We conducted retrospective analysis of line lists obtained from county disease surveillance coordinator in Busia county. Data was analyzed using Microsoft Excel 2010.
Results: In 2016, 52 villages in Bunyala sub-county and one village in Samia sub-county reported cholera outbreaks with a total of 107 cases including six deaths. This gave an overall case fatality rate of 5.6% exceeding the mean CFR of 1% which is acceptable by WHO. Out of the 53 villages, Khainga recorded the highest number of cases nine (8.4%), Lunyofu six (5.6%), Siginga six (5.6%) and Khukunda five (4.6%). The age specific attack rate was highest among individuals 14 years of age and above 62 (58%), 5-14 years 32 (29%) and below five years at 13 (12%). Females were the most affected than males at 59 (55%) and 48 (45%) cases respectively. The epidemiological curve showed peaks on the 4th Feb (18 cases) and 6th (10 cases).
Conclusion: Our study showed a cholera outbreak that grew in magnitude and spread to involve Bunyala North, West and Magombe central in Bunyala sub-county. It also showed potential endemicity of cholera in the villages bordering water bodies i.e., Khainga, Siginga, Lunyofu and Khukunda. Therefore, there is a need for a harmonized, coordinated approach to cholera outbreaks through effective surveillance and response with emphasis on training and motivating frontline healthcare workers towards timely detection and response as well as proper documentation.
Biography:
Shahryar Eghtesadi completed his Bachelor Degree in Nutrition Science and Food Chemistry in 1975, at Shahid Beheshti University of Medical Sciences, Tehran; MSPH Degree in Nutrition in 1977 at Tehran University of Medical Sciences, Tehran and PhD in Nutrition in 1985 at University of California at Davis (UCD), USA. He served as Visiting Scientist in USDA Human Nutrition Research Center on Aging (HNRCA), Boston, USA (1994-1995); Full Professor of Tabriz, Iran and Tehran University of Medical Sciences and currently serves as Professor of Azad University, Science & Research Branch. He was the Chair of Departments of Nutrition and Biochemistry, Biochemistry & Clinical Nutrition, Public Health Nutrition and Nutrition at aforementioned universities. He served as an Associate Dean and Dean of School of Public Health & Nutrition and School of Public Health of Tabriz and Iran University of Medical Sciences respectively. He has published numerous peer reviewed articles in journals and also edited several books and finally served as Principal Investigator of World Bank Project for Capacity Building in Nutrition in Iran.
Abstract:
High prevalence of TB in Golestan Province in north of Iran motivated us to use supplementation with green tea extract to promote healing. The aim of this study was to investigate the effect of green tea consumption on weight changes, iron status and improving process of pulmonary tuberculosis treatment. This double-blinded randomized clinical trial study was conducted on patients with TB, who were assigned randomly to the green tea group (41 patients) receiving 500 mg catechin of green tea extract and the control group (39 subjects) receiving placebo for two months since the beginning of concomitant anti-TB treatment. Height and weight were measured at first and two and six months thereafter. Demographic, food frequency questionnaires and 24-hour dietary recalls of three non-consecutive days were completed. After obtaining 10 ml of venous blood, hemoglobin (Hb), transferrin, ferritin, total iron binding capacity (TIBC), iron and serum malondialdehyde (MDA) were measured in the beginning and the end of the study. Data were processed using independent and paired t-test, McNemar, Wilcoxon, Kaplan-Meier, Log-rank test Cox regression model and Nutrition 4 software. At the beginning of the survey, two groups were similar according to age, gender and clinical status (p>0.05). Average daily energy intake of patients was 1518±434 kcal, distribution of which was as follow: Carbohydrates 58%, protein 17% and fat 22%.Vitamin D and Zinc intake of patients were less and iron intake was higher than the DRI. Weight changes in both groups of placebo and green tea had tendency of increase with a significant difference at two and six month follows ups (pË‚0.0001). However, there were no significant changes due to intervention compared to placebo. ANCOVA test showed mean difference level (P value) in both groups for Hb, iron, TIBC, transferrin and ferritin as of: 0.004, 0.56, 0.65, 0.38 and 0.16, respectively which means that increase of hemoglobin in the green tea group was significant compared to the placebo group. There was just a 9.2 nmol/ml difference between the two groups for MDA in the beginning of study, which was not statistically significant (p=0.078) whereas, it was increased to 24.8 nmol/ml after the intervention, indicating a significant difference (p<0.001). The decline value was estimated -45.45±14.69 nmol/ml for catechin group and -19.91±18.38 nmol/ml for placebo group. In conclusion, green tea as an adjuvant to TB treatment can reduce MDA concentration and improve hematopoiesis and hemoglobin level, but no significant effect on weight gain compared to placebo group.




